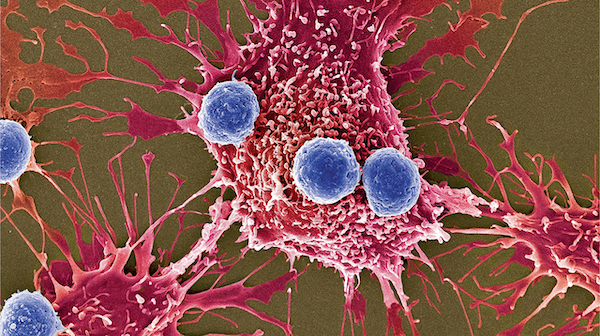
Epithelial ovarian cancer (EOC) remains the most lethal gynecological malignancy in the United States. Implementing immunotherapeutic approaches to treat this disease holds promise, as the ovarian cancer microenvironment is immunologically active; both T cell and B cell infiltration are associated with prolonged patient survival (Zhang*, Conejo-Garcia* et al. N Engl J Med, 2003; Biswas et al. Nature, 2020). However, the microenvironment of ovarian cancer supports unique mechanisms which dampen productive antitumor immunity. This immunosuppressive environment likely explains the typically poor responses to current cancer immunotherapies, and ultimately leads to lethal malignant progression. Thus, the overarching vision of our laboratory is to 1) identify novel immunosuppressive mechanisms in ovarian cancer, and 2) to leverage this knowledge to rationally design the next generation of cancer immunotherapeutics. This vision builds upon my background, where, while working in Dr. Jose Conejo-Garcia's laboratory at Moffitt Cancer Center, we elucidated the mechanism of epigenetic regulation of the immune checkpoint molecule, PD-1, in tumor-infiltrating T cells (Stephens*, Payne* et al. Immunity, 2017). We also have a long-standing interest in butyrophilin and butyrophilin-like molecules (Kumari et al. Int J Mol Sci, 2023), as we recently characterized a unique immune modulatory mechanism of butyrophilin 3A1. In addition to its known role as an activator of Vγ9Vδ2 T cells, we found that butyrophilin 3A1 has the potential to dynamically suppress αβ T cells through an N-glycan-mediated mechanism involving CD45 in ovarian cancer beds (Payne et al. Science, 2020).
Program #1) Identification of novel stress response pathways which impact immune cell function.
Our lab is currently investigating novel stress response pathways which dictate antitumor immune cell activity. It is known that the tumor microenvironment is extremely hostile, with multiple factors contributing to the activation of stress response pathways within tumor-infiltrating immune cells. Such pathways have recently been appreciated as a key regulators of antitumor immunity; in fact, our collaborators have demonstrated that the IRE1α-XBP1 (Nature, 2018) and PERK-NRF2 (Immunity, 2020) endoplasmic stress (ER) response pathways drive immune suppressive mechanisms in cancer; impacting both T cells and myeloid cells. However, our understanding of the array of stress response mechanisms within the tumor microenvironment and their impact on antitumor immunity remains in its infancy. Thus, a major focus of our lab is to understand how novel ATF4-driven stress responses impact antitumor immune cell activity (e.g., T cells, B cells, and myeloid cells) in the ovarian tumor microenvironment. We seek to understand functional and metabolic consequences of intact stress responses within these immune cells, and investigate the therapeutic potential of these cells against cancer upon our genetic or pharmacologic manipulation of their stress response systems.
Program #2) Characterize mitochondrial stress response pathways that drive tumor cell evasion of antitumor immunity
It is now appreciated that the ability of tumor cells to adapt to local environmental stress can facilitate their survival and progression (Payne. Semin Cancer Biol, 2021). Our preliminary data suggest that ineffective or damaged responses to mitochondrial stress response signaling impairs this adaptation feature, and renders tumor cells that are more susceptible to T cell-mediated killing. Through a variety of biochemical and proteomics-based approaches, our lab is beginning to unravel how disrupted mitochondrial stress responses promote 1) enhanced immunogenic tumor cell death, and 2) unfettered tumor cell-derived type I interferon signaling which elicits effector CD8+ T cell infiltration into ovarian tumor beds. We are also currently investigating hypoxia and platinum-based chemotherapeutics as potential drivers of this mitochondrial stress response in order to gain further insight into these understudied systems in ovarian cancer. We anticipate that the knowledge attained in this research program will provide the rationale to develop small molecule inhibitors to target key molecular players in the mitochondrial stress response pathway, as well as predict therapeutic responsiveness in patients harboring deleterious polymorphisms within this signaling pathway. It is expected that this approach will enhance antitumor immune cell activity and will synergize with current cancer therapeutic approaches.
To pursue these studies, we utilize unique genetically engineered mouse models, CRISPR/Cas9 screening techniques and targeted gene ablation, transcriptomic, proteomic, and metabolomics-based approaches, as well as clinical specimens and collaborative efforts.

Payne Laboratory Staff

