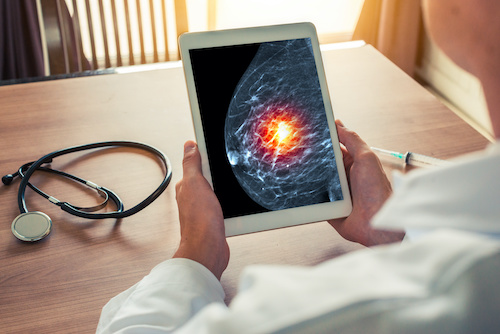
New Brunswick, N.J., September 21, 2021 – Bruce Haffty, MD, MS, chair of Radiation Oncology and associate vice chancellor for Cancer Programs at Rutgers Cancer Institute of New Jersey and system director of Radiation Oncology at RWJBarnabas Health, treated a breast cancer patient with proton therapy which is a unique type of radiation treatment that can precisely target and deliver high radiation doses to a tumor to kill cancerous cells. The patient, who was in her late 30s and in the early months of her first pregnancy while facing a second breast cancer diagnosis, received radiation therapy in her prior diagnosis. Thus, proton therapy was the best option to treat the impacted area while surrounding tissue previously irradiated was spared additional radiation.
Rutgers Cancer Institute and the Laurie Proton Therapy Center at Robert Wood Johnson University Hospital New Brunswick, an RWJBarnabas Health facility, are one of only two programs in the state to offer this select form of treatment. Proton therapy has seen rapid growth in recent years and can be beneficial for select breast cancer patients by minimizing damage to nearby tissue and critical organs. A recent consensus statement from the non-profit professional society Particle Therapy Cooperative Group Breast Cancer Subcommittee, assessed the data available to the radiation oncology community of proton therapy for breast cancer, and provides expert consensus recommendations on indications and technique, and highlights ongoing clinical trials cost-effectiveness analyses and key areas for future research. Dr. Haffty shares some insight about the work published in the May 2021 edition of International Journal of Radiation Oncology Biology Physics (DOI: 10.1016/j.ijrobp.2021.05.110).
What are some of the benefits of proton therapy for breast cancer treatment?
Proton therapy is not offered for the majority of patients with breast cancer. However, there are some circumstances where there may be a benefit. Patients who have previously received radiation therapy and need additional radiation therapy to the same region can possibly benefit, depending on the location of the new problem and details of the prior radiation therapy. There is an ongoing clinical trial at Rutgers Cancer Institute of New Jersey in which investigators will evaluate if there is a benefit in selected patients when the breast and regional lymph nodes require treatment. There are also occasional cases where the radiation dose to the heart or lung with conventional treatment may be higher than ideal and where proton therapy may have an advantage. It is important to understand, however, that the majority of breast cancer patients can be safely treated with conventional radiation therapy.
What are the key recommendations suggested by the authors in the review paper?
The guideline tries to highlight specific situations where proton therapy may or may not have a role in the management of breast cancer. The guideline also provides important information regarding the technical aspects of proton beam delivery that users should be aware of. The guideline also emphasizes the many unanswered questions regarding the use of proton therapy in breast cancer and encourages development and enrollment of patients on clinical trials to address many of these issues.
What’s next for proton therapy research?
With the increasing proton beam facilities throughout the world, many clinical trials are ongoing to try to identify clinical situations where proton beam has an advantage over conventional photon radiation therapy. Clinical trials in breast cancer, brain tumors, lung tumors, esophageal and other gastrointestinal tumors, prostate, gynecologic and other malignancies are all undergoing active clinical trials using proton beam therapy.
The technology of proton beam is also continuously advancing to facilitate rapid, safe and effective delivery of proton beam therapy for patients. Another area of research using proton beam is referred to as FLASH therapy, where the delivery rate of radiation is significantly increased such that the dose is delivered in a fraction of a second, compared with minutes. This rapid delivery has been associated with reduced toxicity to the normal tissues in the radiation field and is currently under investigation for potential clinical applications.
Author disclosures and additional information can be found here.
For journalists – contact:
Krista Didzbalis
Media Relations Assistant
732-507-8307
krista.didzbalis@rutgers.edu
For patient appointments/inquiries – contact:
844-CANCERNJ (844-226-2376)

