
By: Domonique Noel
According to the National Cancer Institute, cancer is defined as “...a disease in which some of the body’s cells grow uncontrollably and spread to other parts of the body” (2021). Although it is not often talked about, cancer can have a significant impact on a person’s body image and sexuality. Body image refers to a person’s perception of the integrity of their physical body (Hungr et al., 2017), and is often tied to one’s internal sense of femininity or masculinity. After undergoing chemotherapy and other cancer treatment procedures, it can have an impact on sexual functioning, including vaginal pain and dryness among women, erectile dysfunction in men, as well as loss of sensation and lowered self-esteem among both genders (Hungr et al., 2017 & Schover, 2018).
As stated in the Journal of Adult Women’s Health and Medicine, over 60% of cancer survivors experience sexual dysfunction, but less than 25% seek professional advice or assistance (Schover, 2018). Among women who have faced a breast cancer diagnosis and undergone a mastectomy, many experience skin damage and discoloration from chemotherapy radiation, and the resulting psychological distress and anxiety from feeling physical shame around having a different body (Hungr et al., 2017). Among cervical cancer survivors, chemotherapy often causes a decline in estrogen and testosterone levels, resulting in lower libido and arousal, tissue fragility, and fatigue (Hungr et al., 2017). Experiencing changes in sexual image and functioning can have an impact on the quality of a person’s romantic or intimate relationship, due to the feeling that one is ‘less of a woman’ (Hungr et al., 2017) and the stigma around discussing changes in sexuality with one’s partner and/or medical provider (Schover, 2018).
Like women who have overcome cancer, male cancer survivors face changes in their bodies, self-image and relationship quality. Among men who have faced a prostate cancer diagnosis, prostate cancer surgery often results in the reduction of the length of the penis and in erectile dysfunction (Laursen, 2016). This can negatively impact one’s internal sense of masculinity and libido (Laursen, 2016). Numerous men often report feeling uncomfortable initiating sexual intimacy, and the need to plan and prepare for sexual activity (Laursen, 2016). In many cases, people have navigated changes in sexual functioning by redefining how they express their sexuality through showing affection and being close with their partners, as an alternative to sex (Laursen, 2016).
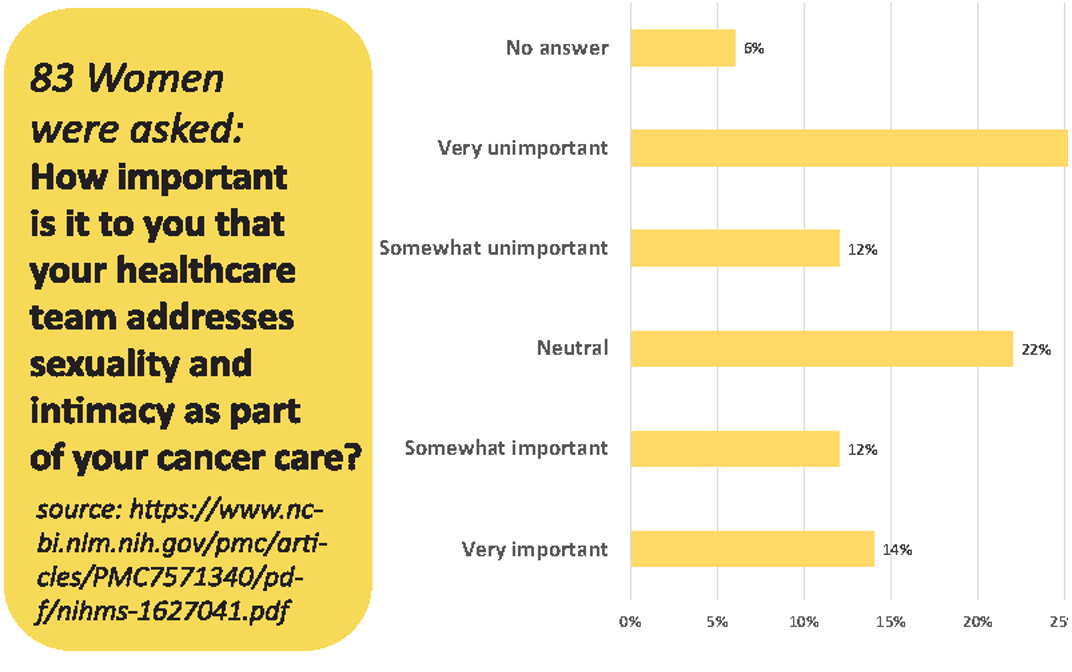
To successfully address the sexual changes experienced among people affected by cancer, it is imperative that providers include questions on sexuality as part of routine cancer care and follow-up visits (Schover, 2018). This can be done by incorporating sex and sexuality experts in the care process (Schover, 2018), so that patients know their options. In addition, patient education materials should include strategies for coping with changes in sexual functioning, including relationship and sex therapy, the use of vaginal lubricants (Hungr et al., 2017), oral medication and/or penile implantation (Laursen, 2016). When inquiring about sexual changes and experiences, it is important to begin by using normalizing statements that encourage patients to express sexual concerns (Hungr et al., 2017). Improving sexual functioning among cancer survivors ultimately starts with changing patient-provider interactions, and prioritizing care from a holistic standpoint which includes sexual health and wellness.
References
- Hungr, C., Sanchez-Varela, V., & Bober, S. L. (2017). Self-image and sexuality issues among young women with breast cancer: Practical recommendations. Revista De Investigación Clínica, 69(2).
- Laursen, B. S. (2016). Sexuality in men after prostate cancer surgery: A qualitative interview study. Scandinavian Journal of Caring Sciences, 31(1), 120–127.
- National Cancer Institute. (2021, May 5). What is cancer? National Cancer Institute. Retrieved January 11, 2022.
- Schover, L. R. (2018). Sexual quality of life in men and women after cancer. Climacteric, 22(6), 553–557.
- Casey M Hay, Heidi S Donovan, Erin G Hartnett, Jeanne Carter, Mary C Roberge, Grace B Campbell, Benjamin E Zuchelkowski, Sarah E Taylor. Sexual Health as Part of Gynecologic Cancer Care: What Do Patients Want? Int J Gynecol Cancer. 2018 November ; 28(9): 1737–1742.

