Story by Mary Ann Littell • Portraits by John O'Boyle View the complete magazine | Subscribe to Cancer Connection
See the full video
View more patient stories at cinj.org/patientstories
Oncologists all share stories about exceptional responders—the small numbers of patients who have a successful, long-lasting response to a treatment that’s failed countless others. It almost seems miraculous.
Cancer survivor Marcia Bird is one of them. In 2011, she was treated for endometrial cancer, a disease that’s generally curable. But Bird wasn’t so lucky. Following surgery, chemotherapy, and radiation, her cancer returned and metastasized. This recurrence called for a tougher fight. She was referred to Rutgers Cancer Institute of New Jersey, where physicians and researchers worked together to find the right treatment. She enrolled in a clinical trial for an immunotherapy drug: specifically, an immune checkpoint blockade. It worked amazingly well, and her tumors melted away. Today, she continues to do well.
Promising advances in immunotherapy are transforming the way researchers and oncologists think about cancer and treat it. Rather than targeting the cancer itself, immunotherapy redirects the body’s own immune system to recognize and attack the disease. In the past decade, this novel treatment has helped many patients with previously untreatable cancer live longer and even be cured. However, it doesn’t work for everyone.
Building on success stories like Marcia Bird’s, Rutgers Cancer Institute researchers seek to harness the power of immunotherapy. To that end, Rutgers has launched a new initiative to improve the application of immunotherapies for cancer treatment, increase the rate of response, and make these therapies more widely available.
The Cancer Immunology and Metabolism Center of Excellence at Rutgers Cancer Institute is a groundbreaking collaboration between clinical and scientific specialties supporting cancer immunology research across many types of cancer. Initially funded by a generous, anonymous philanthropic gift, the Center of Excellence has a mission to develop new immunotherapies, including a new, major initiative to develop novel cell-based immunotherapies.
While many academic centers are studying the dynamic relationship between the immune system and cancer, the Rutgers Cancer Institute Center of Excellence takes a novel approach, uniting cancer immunology and metabolism under one umbrella. This is significant because research shows that metabolism regulates the ability of the patients’ immune system to recognize and eliminate cancer.
Leading the Way
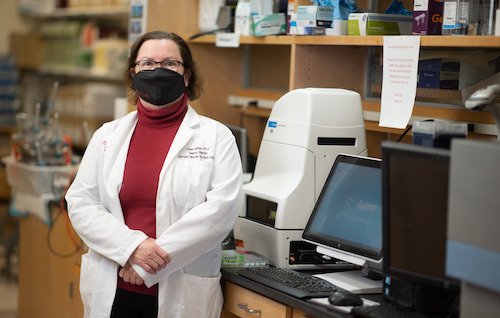
"Our strength in both cancer metabolism research and clinical immunology makes our program unique. Few if any institutions have this capability,” says Eileen White, PhD, Rutgers Cancer Institute of New Jersey deputy director and chief scientific officer and co-director of the Cancer Immunology and Metabolism Center of Excellence at Rutgers Cancer Institute of New Jersey."
“Our strength in both cancer metabolism research and clinical immunology makes our program unique. Few if any institutions have this capability,” notes Eileen White, PhD, the institute’s deputy director and chief scientific officer and a co-director of the Center of Excellence. “By focusing our efforts on determining how tumor metabolism drives growth and suppresses the immune response, we can begin to develop new immunotherapies and make existing immunotherapies more effective.”
Dr. White is a globally recognized expert in the study of metabolism - how cells grow by using energy and nutrients for sustenance - and how it contributes to cancer. In collaboration with research consortium partner Princeton University, her laboratory’s work focuses on understanding the role of metabolism in cancer and how to target metabolic pathways for cancer therapies.
She’s also a principal investigator of a study (see sidebar story) examining the immune response to cancers that feature a high number of mutations. The study uses mouse models with high and low mutation burden to examine how the levels of mutations alter the immune response, and if and how this promotes response to immune checkpoint blockade. This research seeks to explain the exceptional response experienced by Bird and how it can be expanded to benefit more cancer patients.
Co-directing the center is Christian Hinrichs, MD, a world-class expert in cancer immunology and immunotherapy. Recruited from the National Institutes of Health, he joined Rutgers Cancer Institute in January 2021 (see sidebar profile). Dr. Hinrichs is known for discovery and development of new cellular therapies for common types of cancer. With a particular focus on cancers caused by human papillomavirus (HPV), he has discovered personalized cellular and gene therapies for these cancers. His research explores why these treatments work for some patients but not others.
It’s an exciting notion: two outstanding scientists combining their expertise to develop novel and effective therapies for cancer. “Among the strengths of the institute are its strong clinical programs and the diverse patient population it serves from across the state and beyond,” says Hinrichs. “That makes it possible to do the type of research I came here to do. We want to have an ambitious program that takes on many different kinds of cancers.”
The Future of Immunotherapy is Now
As the researchers shared their goals and plans for the Center of Excellence, it’s clear they’ve already developed a strong synergy.

"What’s remarkable about immunotherapy is the way it uses the immune system to specifically target cancer cells and not healthy cells. It has been a real game-changer for sytemic cancer therapy,” says Christian Hinrichs, chief of the Section of Cancer Immunotherapy and co-director of the Cancer Immunology and Metabolism Center of Excellence at Rutgers Cancer Institute of New Jersey.
“What’s remarkable about immunotherapy is the way it uses the immune system to specifically target cancer cells and not healthy cells,” says Hinrichs. “It’s been a real game-changer for systemic cancer therapy for two reasons. First, it creates a very strong attack against cancer. Second, it has remarkably few negative side effects, making it much easier for patients to tolerate than the systemic treatments that preceded it.”
He adds a caveat: “Along with this success comes a dose of reality. Immunotherapy is highly effective in certain kinds of cancers: for example, melanoma and some blood cancers. But the fact remains that most patients who get immunotherapy are not cured. And for many types of cancer, we do not have effective immunotherapy approaches.”
“That challenge is what makes this exciting,” adds White. “We now know how to successfully deploy immunotherapy in a subset of cancers. The research challenge, and the clinical challenge, is to learn how to make this therapy more broadly applicable to more patients and different tumor types. We’re building a group of scientists to tackle this unique aspect of cancer biology. With Christian as our first recruit, we will be adding physician-scientists and immunology-immunotherapy faculty.”
Two exciting breakthroughs in cancer immunology are receiving plenty of attention right now. One is immune checkpoint blockade therapy, a type of immunotherapy that makes tumor cells more susceptible to immune attack. “In simple terms, this therapy is based on taking the brakes off the T cells,” says Hinrichs. “The brakes are negative signals that inhibit the T cell activity. You take the brakes off the T cells so they can attack the tumor.” The second approach is cellular immunotherapies such as adoptive cell transfer. An example of this is chimeric antigen receptor (CAR) T-cell therapy, where a patient’s T cells are extracted and genetically engineered to attack and kill cancer cells.
Both therapies are currently offered to patients at Rutgers Cancer Institute. As the state’s only National Cancer Institute-designated Comprehensive Cancer Center, the institute is a leader in cancer immunology, in the lab and the clinic. It is one of only two sites in New Jersey to offer CAR T-cell therapy. Additionally, a robust clinical trials program is in place, currently offering 74 cutting-edge studies in immune oncology.
Leveraging Hinrichs’ expertise in tumor immunology with White’s knowledge of cancer metabolism, research within the Center of Excellence will help scientists understand why some patients respond to cancer treatments while others do not, and will lead to the development of clinical trials to test novel cancer treatments.
Lending his Expertise
Christian Hinrichs, MD, recently began his role as Chief of the Section of Cancer Immunotherapy and Co-Director of the Cancer Immunology and Metabolism Center of Excellence. Dr. Hinrichs, whose expertise is immunotherapy exploration, was recruited from the National Cancer Institute (NCI) where he served as a tenured Senior Investigator in the Genitourinary Malignancies Branch.

As you learned in the adjacent story, his research focuses on tumor response and resistance with notable accomplishment in the development of cellular therapy for common cancers that begin in epithelial cells – cells in the tissue that line the body’s organs. Hinrichs also has discovered and is developing new treatments for human papillomavirus (HPV)-associated cancers and other types of cancer. This work includes the discovery of genes for T-cell receptors that target HPV. He holds several patents associated with his research and has invented technologies licensed to industry that are being developed as new cancer treatments under his leadership.
“The recruitment of Dr. Hinrichs enables us to build world-class tumor immunology and cancer immunotherapy programs. Leveraging his expertise in tumor immunology with that of Dr. Eileen White in the area of cancer metabolism, the exploration conducted through the Center of Excellence will help us understand why some patients respond to cancer treatments and others do not and lead to the development of clinical trials to test novel cancer treatments,” shares Rutgers Cancer Institute Director Steven K. Libutti, MD, FACS, who is also senior vice president of oncology services for RWJBarnabas Health.
At Focus
An initial area of concentration for the Center of Excellence is on cellular therapies for cancers caused by HPV, Hinrichs’ area of specialty. This wide range of cancers includes almost all cases of cervical cancer as well as cancers of the vulva, vagina, penis, anus, and oropharynx (head and neck).
“The focus of my laboratory is the discovery and development of cellular therapy for common cancers,” says Hinrichs. “CAR T-cell therapy has been effective in blood cancers but more difficult to develop for common solid tumors. We use T cells that target cancers with T-cell receptors (TCRs) rather than CARs because TCRs can attack targets hidden inside the cells, which is the location of the most attractive therapeutic targets. This strategy shows promise and we’re going to study it further.”
He is also exploring a second approach for solid tumors: tumor infiltrating lymphocyte, or TIL therapy. Researchers remove a patient’s tumor and isolate immune system cells that were attacking it. Those cells are grown to large numbers in the lab and infused back into the patient. Hinrichs has successfully used this treatment on four patients with cancers caused by HPV, two of them cervical cancer. While these patients had previously been considered incurable, they remain cancer-free today.
Another ongoing clinical research project involves TCRs Hinrichs discovered while at the NIH. One TCR allows for the targeting of a specific antigen, KK-LC-1, that is expressed by some cervical cancers, gastric cancer, and lung cancer. The second targets Epstein-Barr virus, the cause of several other cancers. Clinical trials are planned to further this research.
“The beauty of Christian’s work is that he’s taking advantage of the fact that approximately 20 percent of human cancers are caused by infection with a virus,” notes White. “The virus has something unique that’s not found on most normal cells. That provides the unique signpost for the T cell to seek out, destroying the tumor.”
“So much revolves around T cells,” Hinrichs observes. “By understanding both the metabolism of the tumor and the immune cells, particularly the T cells, we can improve how well immunotherapy works. This is Eileen’s territory.”
“We’re exploring ways to engineer T cells to be better T cells,” White explains. “You can remove the inhibitory signals on the tumors so the T cells can see the targets, or you can activate different immune cell populations on the tumor microenvironment to have more anti-tumor activity. There are many ways to improve the way the immune system is able to react and eliminate the tumor.”
A Resource to make it Possible
Manufacturing cellular therapies involves collecting blood cells, modifying them to produce a more vigorous attack on cancer cells, and then re-injecting them into the patient. These may be certain types of immune system cells, including a subgroup of T cells capable of killing tumor cells. They may also be tumor cells that have been re-engineered to induce an attack by the immune system. These therapies are typically made in a Good Manufacturing Practices (GMP) facility. The FDA has established stringent regulations for GMPs to ensure the quality of the manufactured therapies.
One of the most exciting aspects of the Center of Excellence is the fact that it has a GMP facility to support investigator-initiated clinical trials. “A GMP facility is absolutely critical for what we do,” says Hinrichs. “It enables us to produce personalized cell therapy products for each patient right here. This makes so much patient-based research possible, allowing us to work in that cutting-edge, personalized therapy space where we can actually discover and develop new cancer therapies at Rutgers Cancer Institute that no one can do anywhere else.”
With two strong leaders and outstanding clinical research, patient care, and technology, the Center of Excellence is poised to lead the immunotherapy revolution and transform cancer treatment.
“A primary goal, even the main mission, is to make immunotherapy more effective, and applicable to more types of cancer,” says Hinrichs. “You could say we want to make exceptional responders out of every patient.”
Fueling the Future
Philanthropy is fueling the launch and progress of the Cancer Immunology and Metabolism Center of Excellence at Rutgers Cancer Institute of New Jersey. The transformational $25 million anonymous gift that launched the Center of Excellence is the largest single donation in the history of the Cancer Institute. In total, the Center of Excellence is a $50 million effort and the generous lead gift has inspired others to support this amazing work as we work to raise the additional $25 million.
As Dr. Hinrichs and Dr. White build their team, additional philanthropic support in the form of start-up funding and endowed chairs will help them attract the best and brightest minds to their team. Such support also will provide the most advanced technology and tools in the combined research cores fueling the pursuit of innovative, high-impact research ideas as they seek the next breakthrough cancer treatments and preventions.
For example, Pat Devitt Risse, PharmD, PHARM’85,’93, donated to support pilot research funding after meeting Dr. White, noting, “Dr. White’s work is exciting and innovative. The combination of cancer metabolism and cancer immunology is a unique approach that places Rutgers Cancer Institute at the forefront for developing new cancer therapies, and pilot funding allows them to pursue new ideas that can turn into significant discoveries.”
If you are interested in supporting the Cancer Immunology and Metabolism Center of Excellence at Rutgers Cancer Institute, please contact the Rutgers Cancer Institute Development Office at cinjdevelopment@ruf.rutgers.edu.

